Maternal mortality in the U.S. has become a pressing concern, as the country continues to report the highest rates of pregnancy-related deaths among high-income nations. Alarmingly, recent studies reveal that over 80 percent of these fatalities are preventable, yet the rates have steadily increased in recent years, particularly during the COVID-19 pandemic. Disparities in maternal health outcomes persist across different racial and ethnic groups, showcasing significant inequities within the healthcare system. Addressing these healthcare system inequities is crucial not only for improving maternal health disparities but also for ensuring women receive adequate postpartum care. With effective strategies and a focus on preventable maternal deaths, there is hope for significant improvements in maternal health in the U.S.
The issue of maternal mortality indicates a critical failure in the reproductive health framework across the United States. As the nation grapples with unacceptably high rates of deaths related to pregnancy and childbirth, there is an urgent need to assess the underlying factors contributing to this crisis. Systemic challenges, such as inadequate prenatal care and postpartum support, alongside stark health disparities among different demographics, highlight the complexities of ensuring safe maternity experiences. Furthermore, the troubling rise in preventable maternal deaths calls for an immediate reevaluation of existing healthcare practices and policies. By emphasizing comprehensive and equitable maternal care, we can work toward a future where childbirth is a safe and healthy experience for all mothers.
The Rising Crisis of Maternal Mortality in the U.S.
Maternal mortality in the U.S. has become a pressing public health issue, particularly as recent studies reveal that pregnancy-related deaths continue to rise. Between 2018 and 2022, the nation experienced alarming increases, driven by systemic inequalities and a lack of sufficient postpartum care. With over 80% of these deaths deemed preventable, it begs the question: why does the U.S., a high-income country, lead the world in maternal mortality rates? This rise is not only a statistic but a call for immediate action to address the disparities affecting various socio-economic and racial groups across the states.
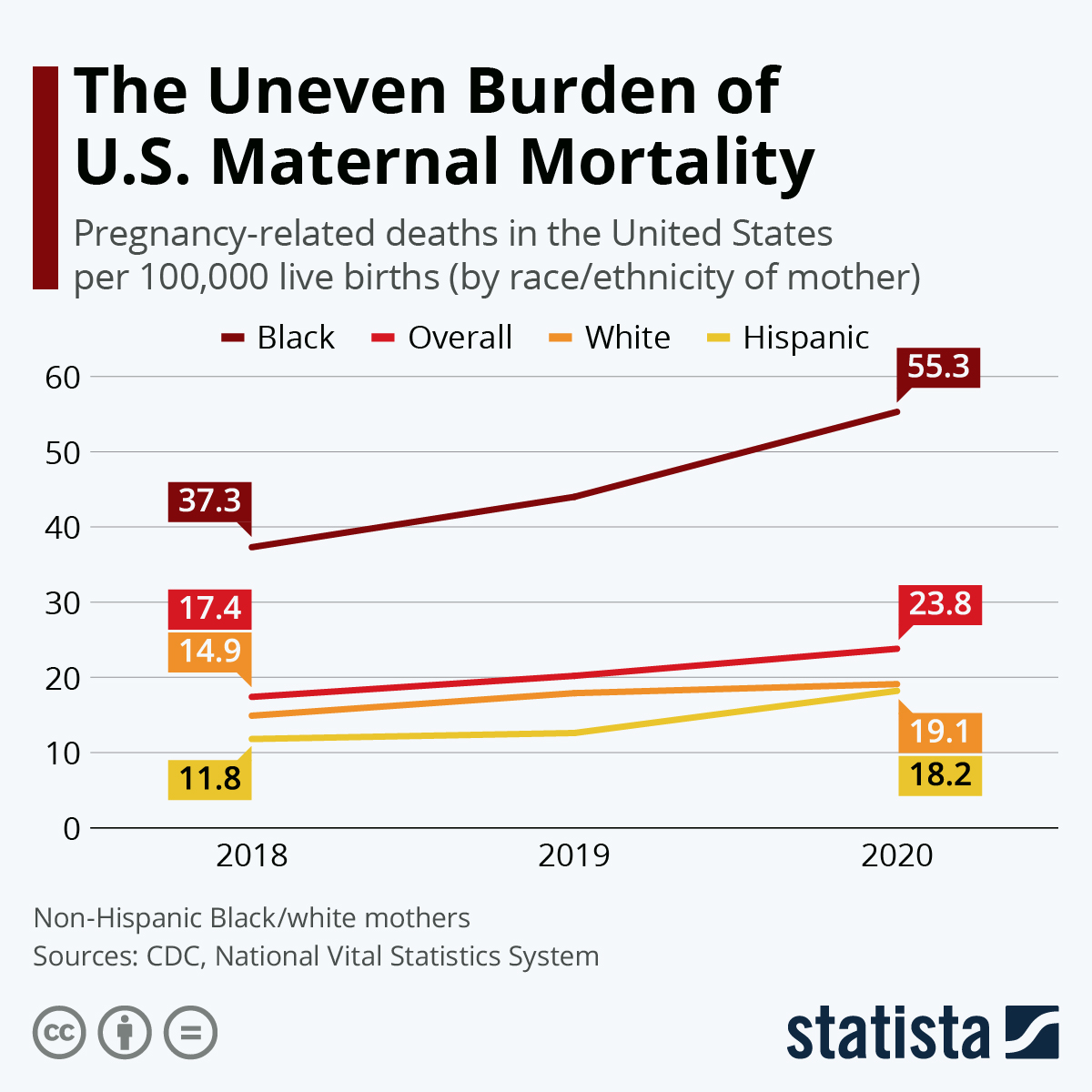
Research indicates that American Indian, Alaska Native, and non-Hispanic Black women face the most significant risks with mortality rates shockingly higher than those of white women. These numbers highlight the urgent need to implement effective policies that ensure equitable access to high-quality maternal healthcare, especially in states where disparities are most pronounced. Addressing these issues through improved data collection and targeted public health initiatives remains essential in combating this ongoing crisis.
Understanding Maternal Health Disparities
Maternal health disparities are deeply rooted in a complex mix of socio-economic factors, access to quality healthcare, and systemic biases inherent in the U.S. healthcare system. The patchwork nature of healthcare provision often results in ‘maternity care deserts,’ where access to prenatal and postpartum services is severely limited. These disparities are further exacerbated by issues such as racial discrimination within the healthcare framework, leading to poorer health outcomes for marginalized communities. By identifying and addressing the social determinants of health, we can better understand the root causes of these disparities and move towards solutions.
It is critical to acknowledge that societal factors play a significant role in maternal health outcomes. Economic instability, lack of education, and insufficient health insurance coverage contribute to the inequalities observed across different groups. Hence, tackling maternal health disparities requires a holistic approach that includes policy reforms, community support systems, and education initiatives aimed at empowering women across diverse backgrounds.
Preventable Maternal Deaths: A Call to Action
Despite advancements in healthcare, the U.S. continues to face a staggering number of preventable maternal deaths. Emerging research reveals that clear strategies could drastically reduce these deaths if implemented effectively. For instance, a concerted effort to improve prenatal care accessibility and ensure follow-up postpartum services for all mothers could significantly enhance maternal health outcomes. It is crucial for policymakers to prioritize maternal health by allocating resources to improve the quality of care delivered during and after pregnancy.
Additionally, community engagement and education are essential components in preventing maternal deaths. By empowering local health organizations and increasing awareness about maternal health issues, we can promote preventive measures that save lives. This could involve providing comprehensive training for healthcare providers to recognize early warning signs and address the unique needs of different populations, ensuring that every woman receives the care she needs at every stage of her pregnancy.
The Importance of Extended Postpartum Care
One of the significant findings from recent studies is the recognition of late maternal deaths that occur between 42 days and one year postpartum. Many healthcare systems overlook this crucial period, focusing predominantly on the first few weeks after birth. It is imperative that we broaden the scope of maternal care to include extended postpartum support to ensure women’s health is continuously monitored and managed. This approach addresses complications that can arise after the typical postpartum checkup, which often leads to preventable fatalities.
Extending postpartum care also involves creating supportive infrastructures within communities that can assist new mothers, such as mental health resources and education on recognizing potential health issues. By bridging these gaps in care, we can create a more comprehensive maternal health paradigm that acknowledges the entirety of the reproductive journey, reducing late maternal mortality rates and promoting healthier outcomes for mothers.
Innovative Solutions for Improving Maternal Health Outcomes
Innovations in maternal healthcare can dramatically shift the current landscape of maternal mortality in the U.S. Technologies such as telehealth and remote monitoring tools can offer pregnant women, particularly those in rural or underserved areas, access to vital healthcare services without the need for extensive travel. By leveraging digital health solutions, we can create more inclusive healthcare experiences that cater to the needs of a diverse maternal population.
Additionally, implementing data-driven policies that focus on real-time monitoring of maternal health trends can help policymakers identify at-risk populations sooner. By utilizing predictive analytics, healthcare providers can tailor interventions based on specific community needs, making strides towards reducing preventable maternal deaths across the board. This proactive stance is essential in reversing the troubling trends in maternal mortality rates.
Policy Recommendations for Enhancing Maternal Care
Addressing maternal mortality in the U.S. requires robust policy reforms that tackle both healthcare inequities and systemic issues within the healthcare system. It’s crucial to advocate for national standards that promote quality care across all states, reducing the significant variations seen in maternal health outcomes. Expanding Medicaid coverage and enhancing access to maternal care services, particularly for low-income families, should be key priorities for lawmakers.
Furthermore, involving community stakeholders in the policymaking process can lead to more personalized and effective maternal care solutions. By fostering partnerships between healthcare providers, local organizations, and policymakers, we can develop comprehensive care strategies that cater to the unique challenges faced by mothers in diverse communities. This collaborative approach can lead to long-lasting improvements in maternal health.
The Role of Healthcare System Inequities
Systemic inequities in the U.S. healthcare system significantly contribute to the disparities in maternal mortality rates among different racial and ethnic groups. These inequities can manifest as barriers to accessing healthcare services, discrimination in treatment, and a lack of culturally competent care. Addressing these issues requires a multifaceted approach that includes training healthcare providers to recognize and combat their biases while also ensuring that maternal health policies reflect the needs of all populations.
In addition to training and awareness, there needs to be a strong push for healthcare reforms that dismantle these inequities. This could include increasing funding for community health centers that serve underrepresented populations and expanding outreach programs that educate women about their rights to quality care. Such systemic changes could pave the way for a more equitable healthcare system, ultimately leading to better maternal health outcomes.
Research Funding and its Impact on Maternal Mortality
The call for increased research funding in maternal health is imperative if the U.S. hopes to reverse its alarming maternal mortality rates. Historical funding cuts have stifled advancements in understanding and improving maternal health outcomes, leaving significant gaps in knowledge. Investing in research that focuses on maternal health disparities and effective interventions can lead to evidence-based practices that save lives.
Moreover, creating a dedicated funding stream for maternal health research can help facilitate long-term studies that track outcomes over time, offering invaluable insights into the effectiveness of various policies and programs. By prioritizing research, we are not only addressing immediate concerns but also laying the groundwork for sustainable improvements in maternal health care delivery.
Empowering Women through Education and Resources
Education plays a crucial role in empowering women to take charge of their maternal health. By informing women about the potential risks associated with pregnancy and childbirth, healthcare providers can encourage proactive measures that can lead to better health outcomes. Health education programs should emphasize the importance of regular checkups, recognizing warning signs of complications, and understanding available resources.
Additionally, providing women with access to comprehensive resources, including mental health support and community services, greatly enhances their overall wellbeing during and after pregnancy. Creating a supportive network that surrounds women with the necessary tools and knowledge will ultimately contribute to lowering maternal mortality rates and improving health for future generations.
Frequently Asked Questions
What are the main causes of maternal mortality in the U.S.?
In the U.S., maternal mortality is primarily caused by chronic conditions, particularly cardiovascular disease, which accounts for over 20% of pregnancy-related deaths. Additionally, complications like hypertension, pre-eclampsia, and issues related to postpartum care significantly contribute to these high rates. It’s essential to acknowledge that more than 80% of these deaths are preventable with improved maternal health care.
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. leads high-income countries in maternal mortality rates, with significant disparities observed based on race and ethnicity. Recent data shows that between 2018 and 2022, maternal mortality rose, underscoring systemic healthcare inequities. For instance, American Indian women experience nearly four times the mortality rate of white women, reflecting deep-rooted maternal health disparities.
What factors contribute to maternal health disparities in the U.S.?
Maternal health disparities in the U.S. are driven by a variety of factors, including systemic bias within the healthcare system, socio-economic inequities, lack of access to prenatal and postpartum care, and the presence of maternity care deserts. These issues disproportionately affect marginalized racial and ethnic groups, exacerbating the risk of pregnancy-related deaths.
Why is postpartum care crucial in reducing preventable maternal deaths?
Postpartum care is vital as nearly one-third of maternal deaths occur between 42 days and one year after pregnancy, highlighting that recovery extends beyond the traditional six-week postpartum checkup. Enhanced postpartum support can lower the risk of complications such as cardiovascular disease, which has become a leading cause of maternal mortality in the U.S.
What role does the healthcare system play in maternal mortality rates in the U.S.?
The U.S. healthcare system, characterized by its fragmented nature and inequitable policies, plays a significant role in contributing to high maternal mortality rates. Improvements in prenatal and postpartum care are needed to address these systemic issues and reduce preventable maternal deaths across different populations.
What initiatives can help reduce maternal mortality and improve maternal health outcomes in the U.S.?
To reduce maternal mortality and improve health outcomes, investments in public health infrastructure, innovative care models, and policies that support maternal health equity are essential. By addressing state-level healthcare disparities and prioritizing comprehensive care during pregnancy and postpartum, we can work towards substantially lowering preventable maternal deaths.
Why are late maternal deaths important in the discussion of maternal mortality?
Late maternal deaths, which occur between 42 days and one year postpartum, represent a critical aspect of maternal mortality that often goes underreported. Understanding and addressing these deaths can lead to improvements in postpartum care, as this period is crucial for addressing ongoing health risks that mothers face long after childbirth.
How has the COVID-19 pandemic impacted maternal mortality rates in the U.S.?
The COVID-19 pandemic has likely exacerbated maternal mortality rates, especially in 2021, when the highest increases were recorded. Factors such as increased stress, healthcare access issues, and potential delays in receiving care during the pandemic have contributed to this concerning trend.
| Key Point | Details |
|---|---|
| Rising Maternal Mortality Rate | The U.S. has the highest maternal mortality rate among high-income countries, which has continued to rise from 2018 to 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths are preventable, highlighting a critical area for improvement in healthcare. |
| Racial Disparities | American Indian and Alaska Native women have the highest mortality rate, with significant disparities across ethnic groups. |
| Impact of COVID-19 | 2021 witnessed the most significant increase in mortality rates likely due to the pandemic. |
| Need for Improved Care | There is a urgent need for better prenatal and postpartum care to mitigate the risk of pregnancy-related deaths. |
| Late Maternal Deaths | Nearly a third of maternal deaths occur between 42 days to one year after pregnancy, indicating the need for longer-term care. |
| Focus on Chronic Conditions | Cardiovascular disease now tops the list as the leading cause of maternal mortality, exacerbated by chronic conditions. |
| Variability by State | State rates vary widely, indicating policy discrepancies that need to be addressed for equitable healthcare. |
Summary
Maternal mortality in the U.S. remains a pressing public health crisis, with rates continuing to rise and significant disparities among racial and ethnic groups. The findings from recent studies emphasize the urgent need for improved prenatal and postpartum care. By focusing on preventative measures, addressing systemic biases, and enhancing healthcare infrastructure, we can work towards drastically reducing the number of preventable pregnancy-related deaths. Investing in public health initiatives and policy reforms is essential to ensure better outcomes for mothers across the nation.